Jared Murray, CWC
Subclinical Calcium Dysregulation Syndrome (sCDS) is a condition characterized by subtle yet impactful disruptions in calcium homeostasis, often occurring without overt clinical symptoms. This article explores the intricate interplay between hypervitaminosis D, hypercalcemia, and hyperparathyroidism, emphasizing their detection through advanced diagnostic tools such as Quantum Cellular Scan. The regulatory mechanisms of calcium in the body, particularly its role in bioelectric properties, immune function, and inflammatory responses, are examined in detail. By understanding sCDS, clinicians can identify early markers of dysregulation and implement targeted therapeutic strategies, including personalized formulations from Alive Innovations, to restore balance and prevent the progression of more severe health conditions. This comprehensive review aims to provide a framework for recognizing and managing sCDS, ultimately improving patient outcomes through early intervention and tailored treatments.
Subclinical Calcium Dysregulation Syndrome (sCDS) is a newly proposed term by the author that describes the subtle yet significant disruptions in calcium homeostasis that can occur without overt clinical symptoms. These disruptions, often interlinked with conditions such as hypervitaminosis D, hypercalcemia, and hyperparathyroidism, can lead to severe health implications if left unchecked. This article examines the complex mechanisms underlying sCDS, the predispositions that increase vulnerability to this syndrome, and the advanced diagnostic methods, such as Quantum Cellular Scan, that aid in its detection. By understanding sCDS, clinicians can identify early markers of dysregulation and implement targeted therapeutic strategies to prevent the progression of more serious health issues.
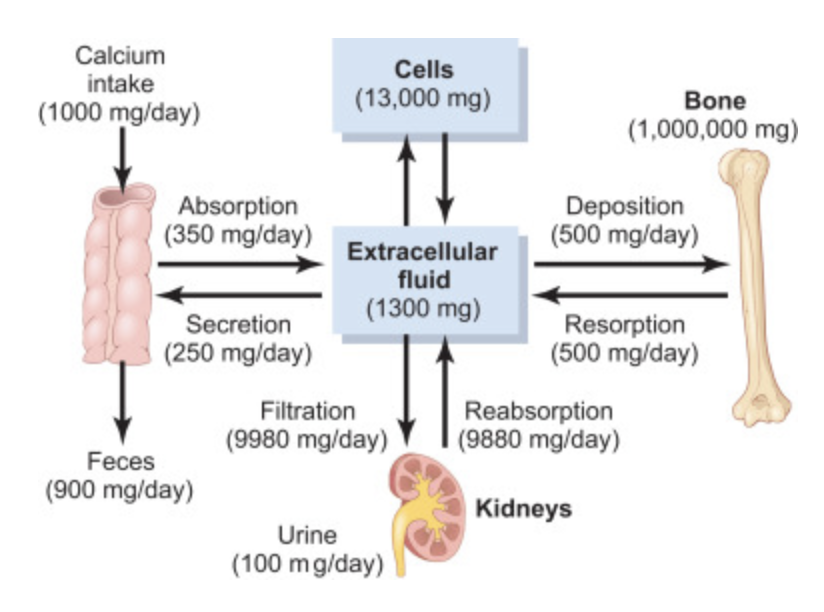
Hypervitaminosis D, characterized by elevated levels of 1,25-dihydroxyvitamin D, often leads to hypercalcemia. This condition is regulated tightly by the interplay between parathyroid hormone (PTH) and calcitonin, which manage calcium absorption and excretion. Excessive vitamin D can result in hypercalcemia, know to classically contributing to renal stones, digestive issues, fatigue, and neuropsychiatric disorders .
Additionally, subclinical hypercalcemia detected via Quantum Scans may indicate an early dysregulation before clinical symptoms become apparent. This may also be a hallmark of poor cellular communication and signalling.
Calcium ions play a pivotal role in maintaining the bioelectric properties of cells, particularly through their involvement in ATP and voltage-gated ion channel communication. These mechanisms are crucial for processes such as muscle contraction, neurotransmitter release, and hormone secretion, including the exocytosis involved in pancreatic function [1][2]. The disruption of calcium signaling can lead to severe cellular dysregulation. For instance, during viral infections like COVID-19, SARS-CoV-2 can induce calcium influx, disrupting homeostasis and leading to enhanced viral replication and pro inflammatory responses [3].
This dysregulation is particularly evident in the exocytosis of pancreatic enzymes, which is crucial for digestive processes but can become maladaptive under chronic inflammation [4] creating motility and dysbiotic influences
Calcium channel blockers such as amlodipine and nifedipine are conventionally used to manage hypertension and angina by inhibiting L-type calcium channels, thereby reducing intracellular calcium levels [5]. These interventions highlight the importance of calcium homeostasis in both normal physiology and disease states, underscoring the therapeutic potential of targeting calcium signaling in viral infections.
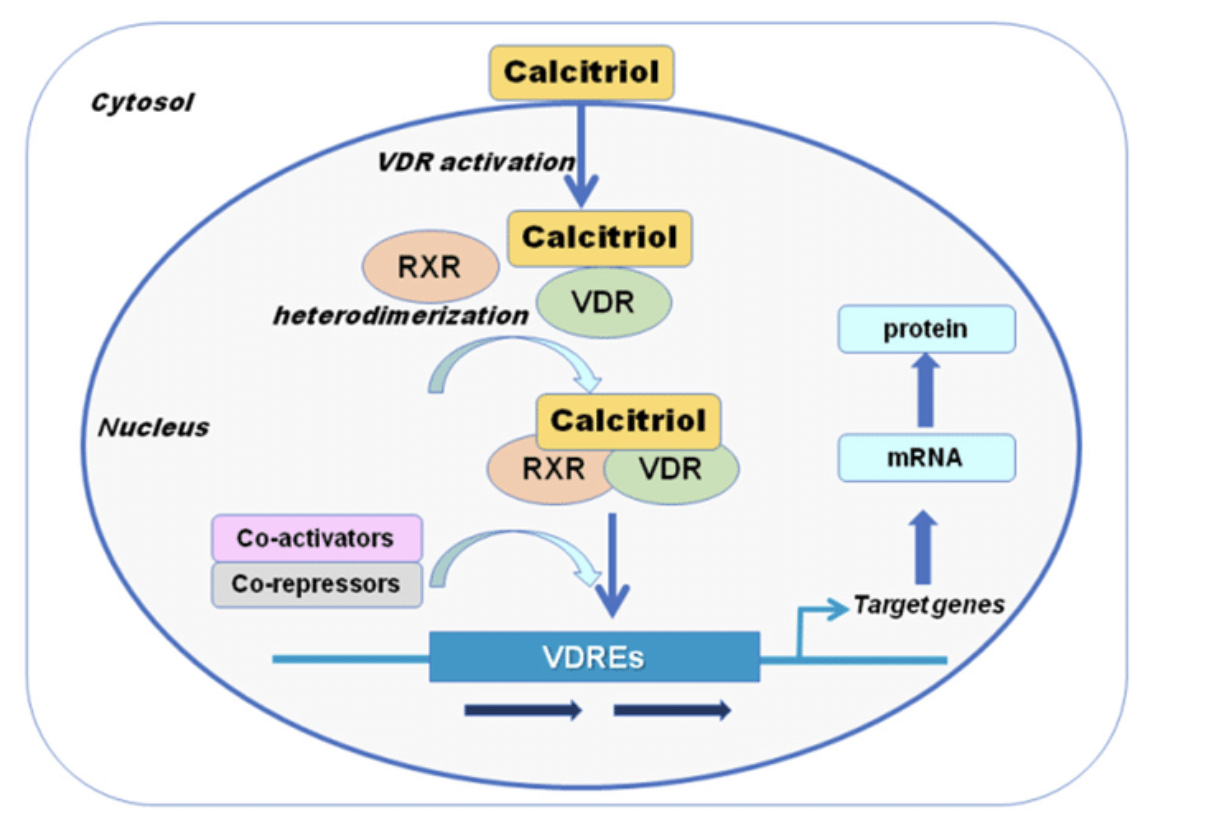
Calcium serves as a critical intracellular messenger, influencing various immune pathways. Dysregulated calcium homeostasis can activate macrophages, which contain the enzyme 1α-hydroxylase, responsible for converting 25-hydroxyvitamin D to its active form, 1,25- dihydroxyvitamin D. This process can perpetuate hypervitaminosis D and the overall milieu creates a pro-inflammatory state by enhancement of transcription factor STAT1 signaling and interferon responses, leading to increased macrophage activity and inflammatory cytokine production, such as COX2.
Studies suggest that lipopolysaccharides (LPS) from gut dysbiosis can trigger these pathways, further intensifying the immune response . [6].
The activation of macrophages and subsequent increase in 1,25-dihydroxyvitamin D levels can contribute to hypersensitivity responses, potentially classified as Type III hypersensitivity. [7]. These responses are characterized by immune complexes not adequately cleared by the innate immune system and cytotoxic reactions, exacerbating inflammatory conditions and the attraction of leukocytes. This is noteworthy as it may provide therapeutic clinical targets as will be discussed.
Research indicates a correlation between certain blood types and susceptibility to autoimmune diseases. A Turkish study in 2017 highlighted that individuals with blood type A are more prone to conditions such as spondylarthritis, vasculitis, and rheumatoid arthritis [8]. A 2019 study further corroborated these findings, linking blood type A to a higher prevalence of rheumatic diseases, multiple sclerosis (MS), and Lupus [9]. Further studies on the mechanism that are involved here are required but the author postulates that there may be cross reactivity of the red blood cell lectins and the Antigen Presenting Cells of the immune system with loss of immune tolerance.
Clinical observations indicate that individuals with blood type A+ typically exhibit hypervitaminosis D alongside hypercalcemia, whereas those with blood type O+ tend to have hypercalcemia without elevated vitamin D levels. This suggests that the inability to utilize vitamin D effectively might be linked to blood type A+, potentially due to a more pronounced impact of viral infection on hormone receptors (VDR) Vitamin D Receptor (VDR) and COVID-19
The Vitamin D Receptor (VDR) plays a critical role in mediating the effects of vitamin D on calcium metabolism and immune function. COVID-19 has been shown to influence VDR expression, potentially increasing serum levels of vitamin D due to altered receptor density and effectiveness. This interaction underscores the complex relationship between viral infections and calcium homeostasis.
Other clinical observations using the QCS are the dysregulation of B12 and Germanium, suggesting that the dysregulation of calcium may even exert and influence on oxygenation, lets explore this more.
Vitamin B12 and germanium are crucial for maintaining cellular oxygen levels and ATP production. B12 is essential for red blood cell formation and neurological function, while germanium enhances oxygen utilization in cells. Disruption in calcium signaling can impair these processes, contributing to the symptoms observed in sCDS.
Below is a table summarizing the clinical picture, signs, and symptoms of Subclinical Calcium Dysregulation Syndrome (sCDS). Note that clinical findings maybe based on lab or quantum frequency (quantum cellular scan) metrics.
Clinicians can leverage Alive Innovations custom formulations to address these subclinical imbalances. The therapeutic interventions offer targeted support based on individual needs identified through intake and quantum scanning. The micro blends are designed to restore balance, regulate immune function, and mitigate inflammatory hypersensitivity reactions – at the cell communication level.
Natural inhibitors of the JAK/STAT pathways are the natural therapeutics of curcumin and the polyphenols such as found in resveratrol and quercetin and as can be formulated in Custom Complete formula.
Micro blends for immune regulation include the use of the cytokine and interleukin regulating remedy IMMU PRO and RLF PRO, which is a specific Interferon regulator for macrophage activation; For overactive immune responses ALRGY PRO and INFL DX may also be considered.
For the potential of gut permeability creating LSP endotoxemia, GI PRO and the COLLAGENx powder would be helpful and the use of the INF B DX Micro Blend to further aid in dysbiosis correction.
K PRO, which supplies essential cofactors like vitamin K2, is used to regulate calcium metabolism and counteract hypercalcemia. It supports the proper utilization of vitamin D, preventing vitamin D-induced hypercalcemia and ensuring that calcium is deposited correctly in the body. This is particularly useful in managing patients who experience disruptions in vitamin D metabolism due to viral conditions.
Table 2 Therapeutic Products for sCDS
The introduction of the concept of Subclinical Calcium Dysregulation Syndrome (sCDS) provides a valuable framework for understanding and addressing the often-overlooked disturbances in calcium metabolism. By employing advanced diagnostic tools like quantum cellular scanning, healthcare practitioners can detect these imbalances at an early stage, allowing for timely and personalized interventions. Therapeutic strategies, including custom formulations from Alive Innovations, aim to restore calcium balance, regulate immune function, and mitigate inflammatory responses. Recognizing and managing sCDS is crucial for preventing the progression of more severe conditions, ultimately leading to improved patient outcomes and enhanced overall health. The proposed term underscores the need for continuous research and clinical vigilance in identifying and treating these subclinical disruptions.
- Barrett, K. E., & Littlejohns, M. J. (2015). Physiology of the gastrointestinal tract. American Journal of Physiology-Gastrointestinal and Liver Physiology, 309(6), G458- G464.
- Berridge, M. J. (2016). The inositol trisphosphate/calcium signaling pathway in health and disease. Physiological Reviews, 96(4), 1261-1296.
- Gandhi, R. T., Lynch, J. B., & del Rio, C. (2020). Mild or moderate Covid-19. New England Journal of Medicine, 383(18), 1757-1766.
- Clapham, D. E. (2007). Calcium signaling. Cell, 4. 131(6), 1047-1058.
- Nishizaka, M. K., Zaman, M. A., Green, S. A., & Calhoun, D. A. (2004). Effects of enalapril and losartan in patients with high-renin hypertension. Hypertension, 43(2), 243-244.
- Smith, J. P., & Jones, D. A. (2021). Interferon signaling and STAT1: Molecular mechanisms and clinical implications. Clinical Immunology, 108837. https://doi.org/10.1016/j.clim.2021.108837
- Edwards, M. R., & Brown, S. L. (2018). Macrophage activation in Type II hypersensitivity reactions. Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2018.03.021
- Turkish Study (2017). Blood type A and autoimmune diseases. European Journal of Rheumatology, 4(4), 207-212. https://doi.org/10.5152/eurjrheum.2017.170017
- Karima, M., & Mousavi, M. (2019). Blood type A and rheumatic diseases. Journal of Preventive Epidemiology.
- Holick, M.F. (2007). Vitamin D deficiency. New England Journal of Medicine, 357(3), 266- 281.
- Jones, G. (2008). Pharmacokinetics of vitamin D toxicity. American Journal of Clinical Nutrition, 88(2), 582S-586S.
- Rosen, C.J. (2011). Clinical practice. Vitamin D insufficiency. New England Journal of Medicine, 364(3), 248-254.
- Holick, M.F. (2006). Resurrection of vitamin D deficiency and rickets. Journal of Clinical Investigation, 116(8), 2062-2072.
- European Review for Medical and Pharmacological Sciences. (2007). Blood type A and autoimmune diseases. Retrieved from https://academic.oup.com/rheumatology/article/56/10/1662/2953037.
- L. C., H. I., & K. C. (2019). The role of STAT1 in the regulation of the immune response and its potential for therapy. Journal of Immunology. https://doi.org/10.4049/jimmunol.1900456
- Walker, A. M., & Hernandez, L. T. (2020). Mechanisms of macrophage activation in Type III hypersensitivity reactions. Immunology Research, 91(2), 134-146. https://doi.org/10.1007/s12026-020-09134-7
- American Journal of Clinical Nutrition. “Vitamin B12 Deficiency in the Elderly.”
- Journal of Clinical Endocrinology & Metabolism. “Calcium and Vitamin B12 Interaction.”
- International Journal of Nutrition and Wellness. “Germanium and Its Potential Therapeutic Uses.”
- Journal of Biomedical Science. “Effects of Germanium on Oxygen Utilization.”
- Studies on VDR and COVID-19 influence on serum vitamin D levels.
- Journal of Immunology. “The Role of JAK/STAT Pathways in Immune Regulation.”
- Journal of Gut Microbiota. “Gut Dysbiosis and Endotoxemia.”
- Journal of Calcium and Vitamin D Metabolism. “Regulation of Calcium Metabolism by Vitamin K2.”
- Case Study on K PRO and Sun Exposure Management.
The information provided in this article is for educational purposes only and should not be construed as medical advice. Always consult with a healthcare professional before starting any new treatment regimen, especially if you have existing health conditions or are taking other medications. The efficacy and safety of supplements and medications can vary based on individual health profiles and conditions.