Jared Murray, CWC
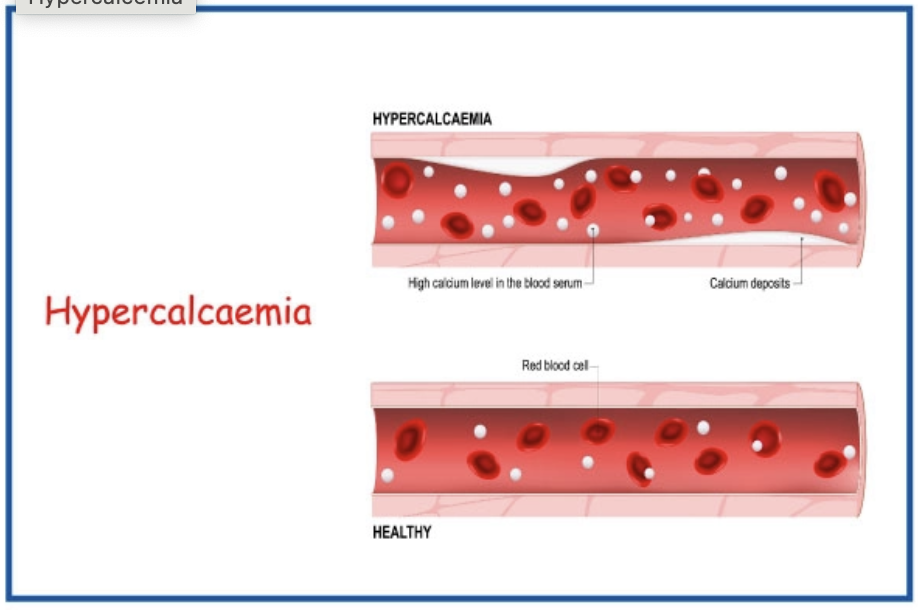
In my recent scans, I have noticed a puzzling pattern of hypervitaminosis D, increased calcium, parathyroid hormone, and the associated influences; this leads me to wonder do we need to re-examine the role of Vitamin D especially with direct or indirect exposure to the COVID spike protein? These cases fit into predominantly two categories. Those with A+ blood type had hypervitaminosis D and typically hypercalcemia, O+ typically just hypercalcemia. In my observations 99% of the time clients fit into these two groups.
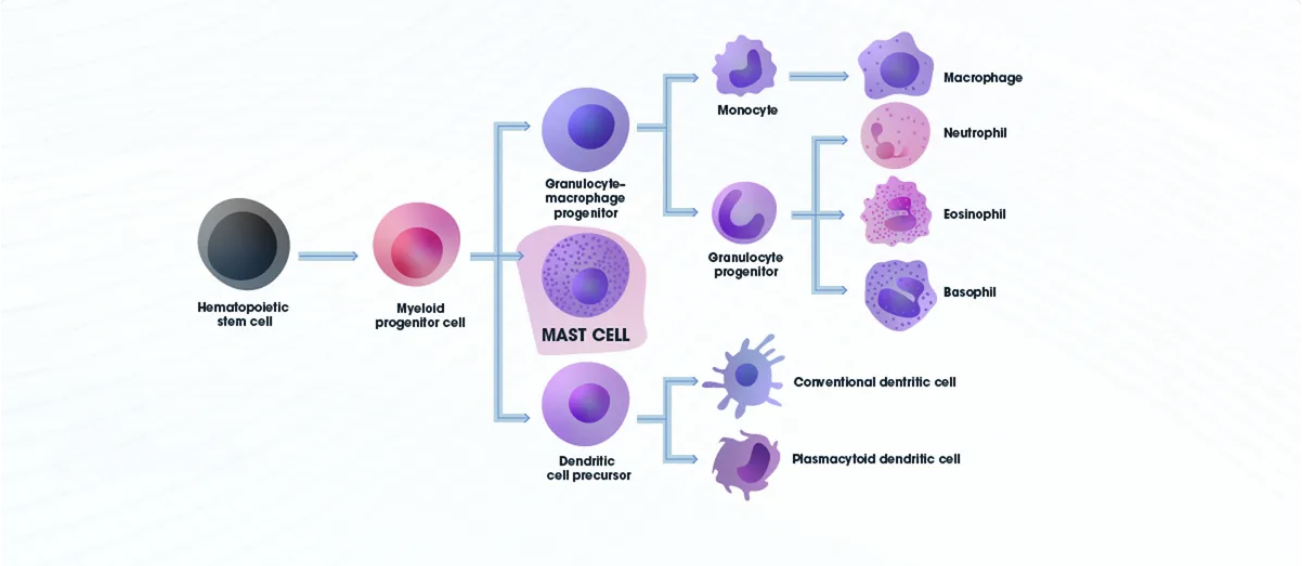
In the early days of COVID, there was much discussion on the deficiency of Vitamin D creating increased morbidity and mortality; the ACE-2 receptor was thought to also be influenced in part possibly allosterically by the Vitamin D cell and nuclear receptors on the macrophages. That lead to people mega dosing on Vitamin D; but that isn’t the whole story… What are the connections between players that may explain the puzzle: the Spike protein, mast cells, and vitamin D.
November of 2020 a group of doctors and mast cell researcher suggested the following: “Much of Covid-19’s hyperinflammation is related to inflammation which MC [mast cell] activation can drive. Drugs with activity against MCs or their mediators have preliminarily been observed to be helpful in Covid-19 patients. PMID: 32920235
None of the authors’ treated MCAS [mast cell activation syndrome] patients with Covid-19 suffered severe infection, and even mortality; Hyperinflammatory cytokine storms in the many severely symptomatic Covid-19 patients may be due an atypical response to SARS-CoV-2 by the dysfunctional MCs of MCAS rather than a normal response by normal MCs. It is a theory that must be tested and researched more.
The mast cells discharge their inflammatory soup and substances such as histamine, leukotrienes, prostaglandins, and cytokines – triggered by several stimuli.
Mast cells are present in most tissues, including the lung, the gut, and the brain (called microglial cells) They were originally recognized for their capacity to kill parasites with the toxic contents of their granules. However, a dysregulated degranulation of mast cells can result in allergy or hyper-inflammation. Mast cells have been suspected to play a role in the severity of COVID-19. In December of 2021, Wu et al. published a study titled SARS-CoV-2-triggered mast cell rapid degranulation induces alveolar epithelial inflammation and lung injury. PMID: 34921131
Interestingly, these researchers could reproduce the effects of the virus on mast cell degranulation with just the Spike protein binding to the ACE2 receptor on mast cells. This makes their findings relevant not only to the impact of COVID infection, but also to the impact of COVID vaccines, which make the body produce the Spike protein for unknown duration of time.
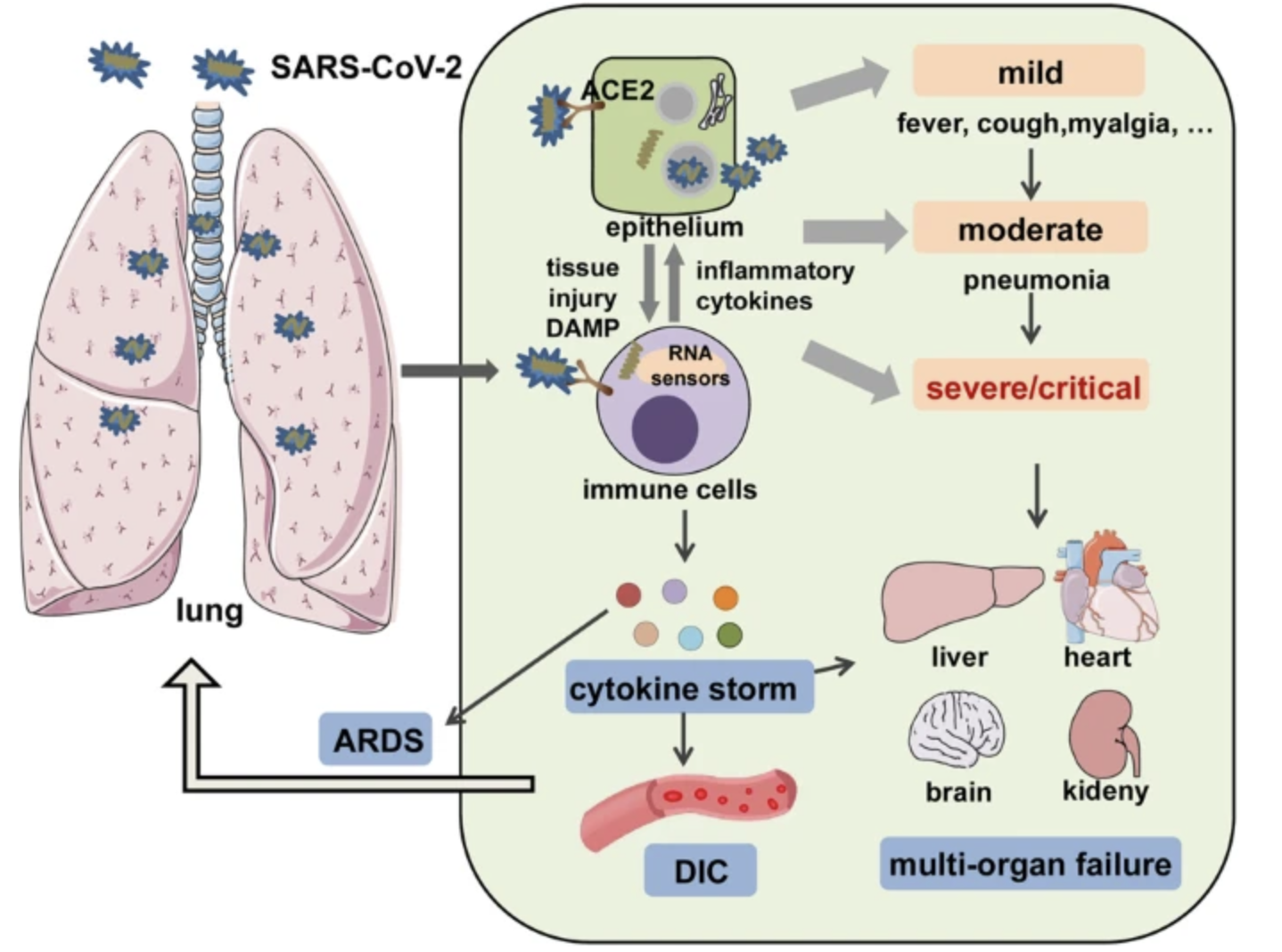
It is this response that can trigger mast cells (via ACE2) and putting some people at risk of severe outcomes. This is especially the case for people, whose mast cells are already destabilized due to environmental exposures, chronic inflammation, or pre-existing conditions.
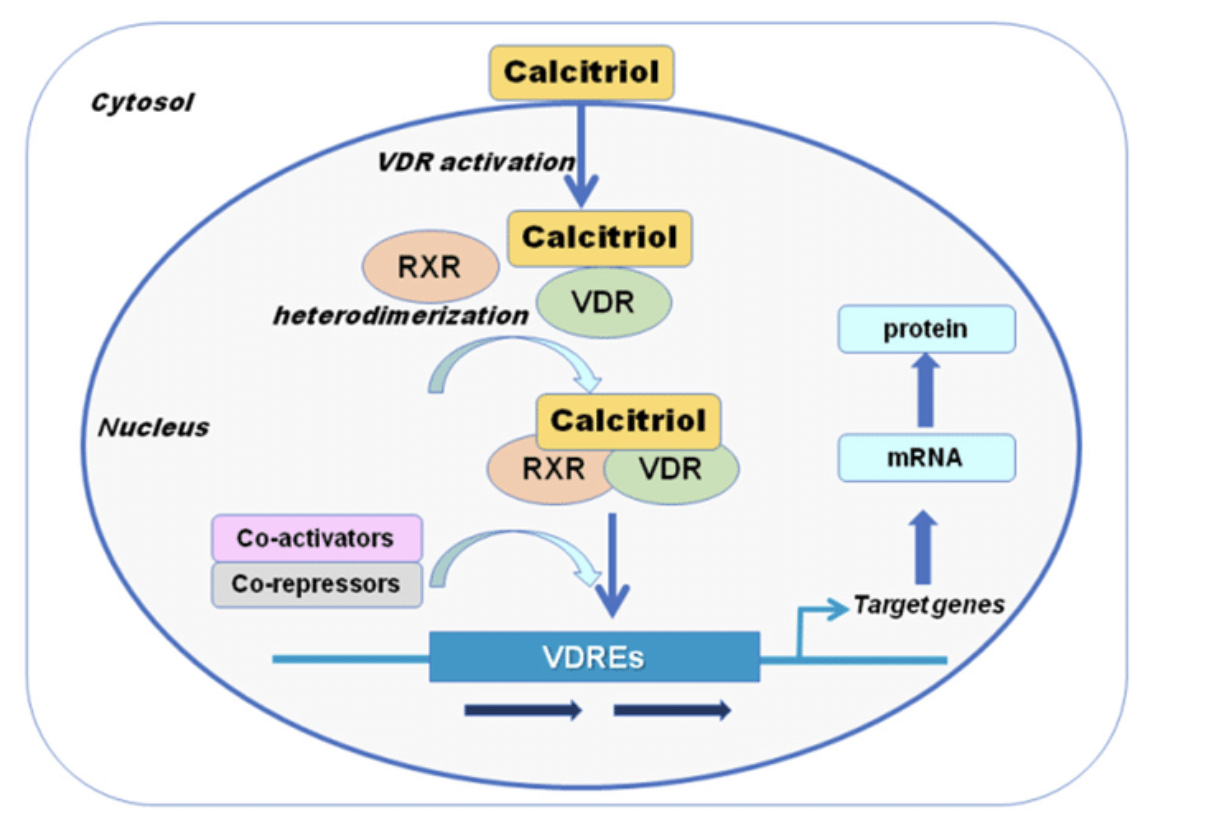
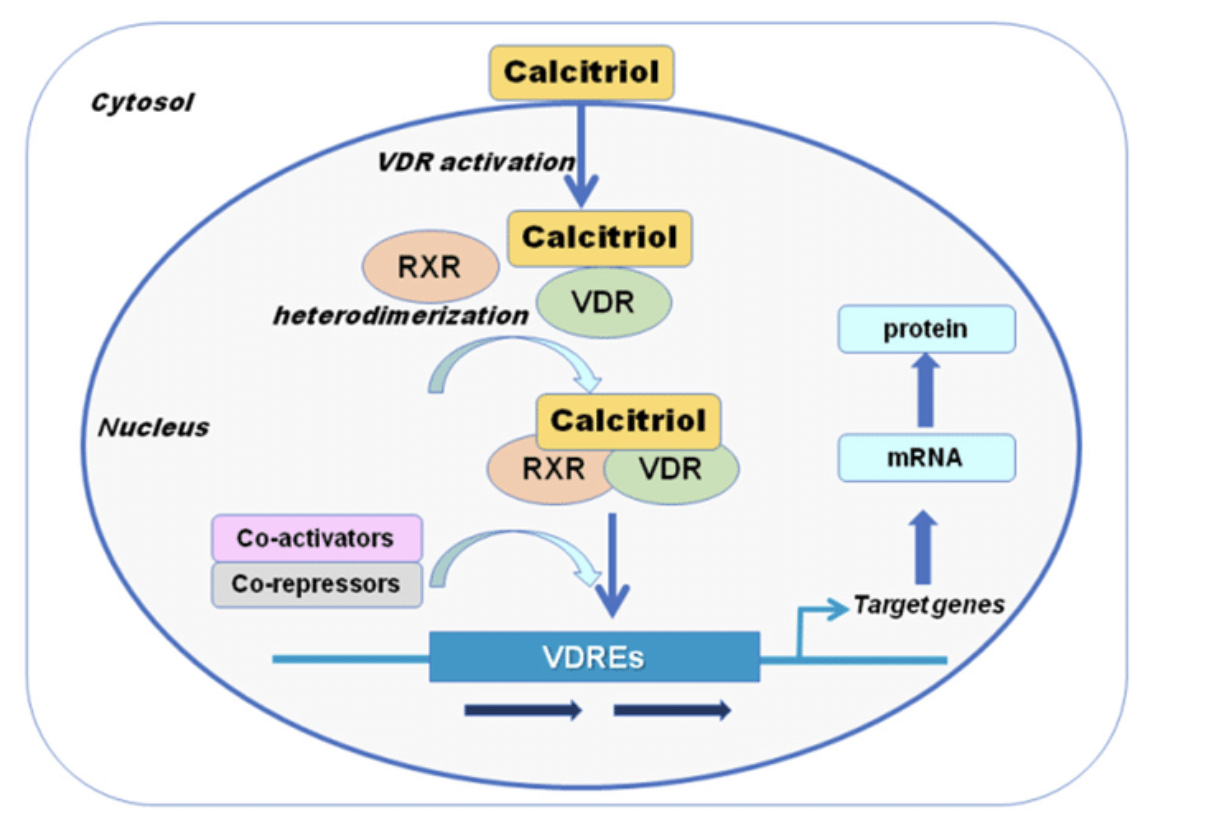
My belief is that the VDR (vitamin D) receptor functions maybe overwhelmed by dysregulated spike protein responses, causing increased levels of Vitamin D in the serum and in QSC scanning causing calcium build up in the body – also known as granulomatous disease. PMID: 33864942
In more than half of these cases clients where NOT consuming vitamin D despite levels being elevated. And based on analysis the client did need vitamin D however could NOT absorb it.
This is a departure for the understanding of Vitamin D deficiency and COVID infection; A 2017 study found that mast cells activate spontaneously in a vitamin D-deficient environment, and the vitamin D levels are inversely correlated with COVID severity, if indeed mast cells are driving it. PMID: 27998003 And pre-existing chronic conditions such as inflammation and obesity are often accompanied by low vitamin D levels.
Maintaining adequate plasma levels of Vitamin D is not simply a matter of dietary intake and sun exposure, but also depends upon the reduction in pollutant, pesticide and glyphosate exposure and a healthy microbiome.
Inflammatory endotoxin LPS, produced by certain strains of gut bacteria, can be responsible for driving chronic inflammation via endotoxemia (increased presence of LPS in the bloodstream). And chronic inflammation depletes vitamin D. The link between LPS and vitamin D degradation has been established in this study, by showing that LPS upregulates vitamin D-metabolizing enzymes, CYP27B1 and CYP24A1, in white blood cells.
Stabilization of mast cells also requires maintaining a healthy gut barrier to prevent LPS (lipo-polysaccharide) leakage into the bloodstream and subsequent vitamin D degradation. So, is it possible that that one answer to the clinical observation of hypervitaminosis D lies in the leaky bowel issue? Made worse by the dysregulated mast cells? These cells themselves can pose a challenge to healing the gut as they contribute to the gut barrier dysfunction, potentially fueling their own destabilization.
In addition, mast cells can degranulate when exposed endocrine-disrupting herbicides, toxicities and power-frequency EMFs maybe even the 5G; possible additives to vaccines can also result in the release of inflammatory mediators from mast cells. And let’s not forget that psychological stress exacerbates mast cells via stress hormones and neurochemicals.
Healing from long-COVID or COVID vaccine injury or preparing to handle COVID exposure uneventfully should include mast cell care. Improve the microbiome and regulate the Vitamin; there are also some food substances known to mitigate their activation; some of the Alive Innovation remedies for consideration are ALRGY PRO, INFL PRO, IMMU PRO, Quercetin, Arginine, Resveratrol, K PRO, and PHOS PRO.
Exposure to Covid seems to cause dysregulation with both vitamin D and by extension calcium in A+ clients. In O+ clients vitamin D dysregulation was not apparently obvious; however, hypercalcemia was apparent.
In both cases symptomatic issues of hypercalcemia were predominate; nausea, stomach issues, GI issues, tired but unable to sleep, wrestles legs, achy joints, vision issues, cloudy thinking, neurotic behavior and more. Supporting calcium using PHOS PRO along with SLK PRO to support kidney function was generally the first approach. In the absence of blood type, we noticed a trend of K PRO matching along with INFL PRO; To assist in binding vitamin D, and support for inflammation reduction respectively.
In my lifetime I have rarely seen Vitamin D toxicity, especially from those that are NOT taking vitamin D. Along with this seeing relatively young clients in 30- 50’s have calcium issues where thyroid and parathyroid function is clinically normal is out of the ordinary.
For those in the wellness industry or may have symptoms like hypercalcemia it would be wise to review the basics. The Spike protein seems to be pervasive in simple observations to me, clearly linked with these conditions causing a Trilogy of Trouble.
The information provided in this article is for educational purposes only and should not be construed as medical advice. Always consult with a healthcare professional before starting any new treatment regimen, especially if you have existing health conditions or are taking other medications. The efficacy and safety of supplements and medications can vary based on individual health profiles and conditions.